mRNA Cell Engineering Enables Rapid Prototyping of Macrophage Gene-Editing Strategies for Cancer Immunotherapy Applications
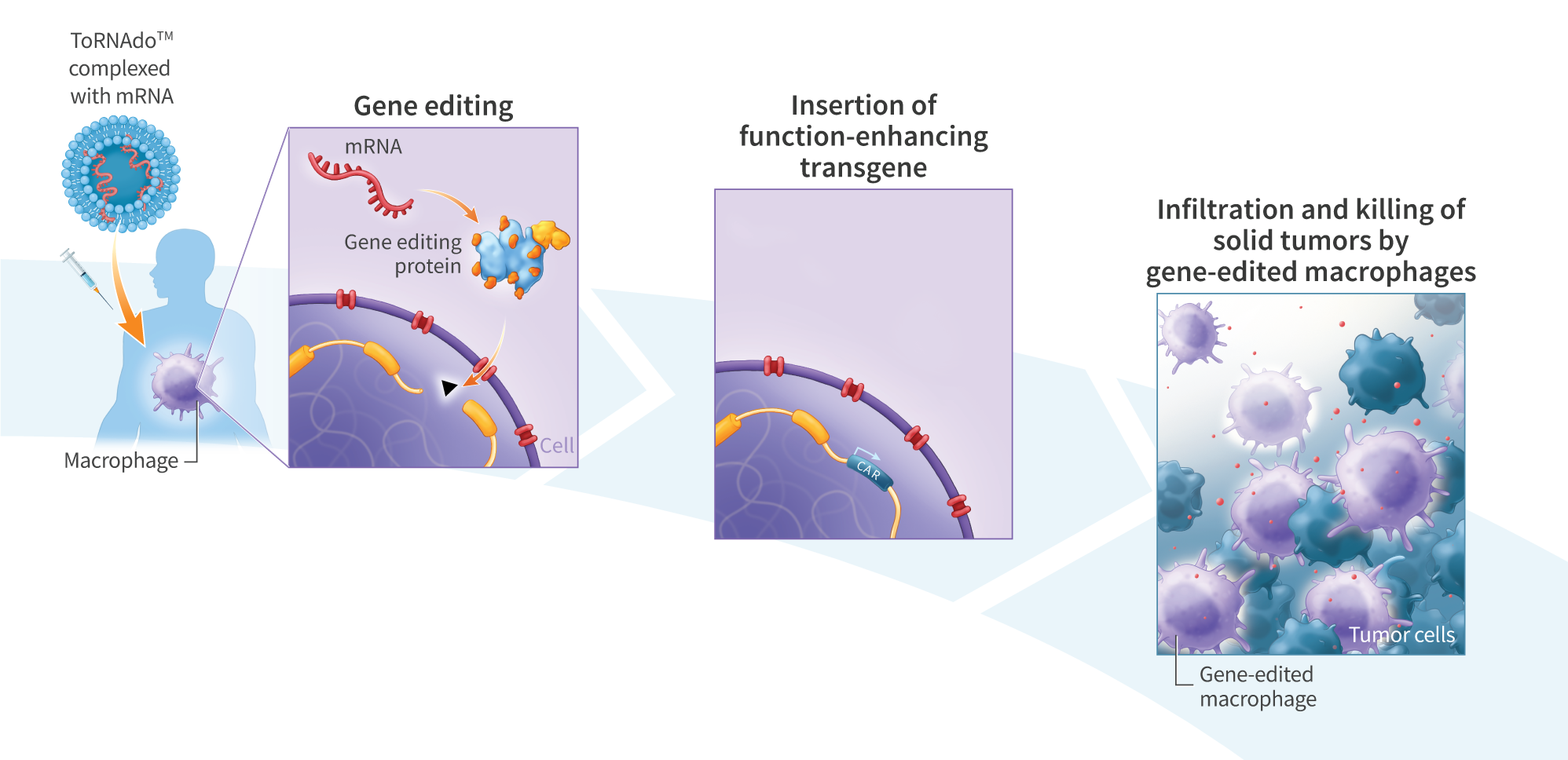
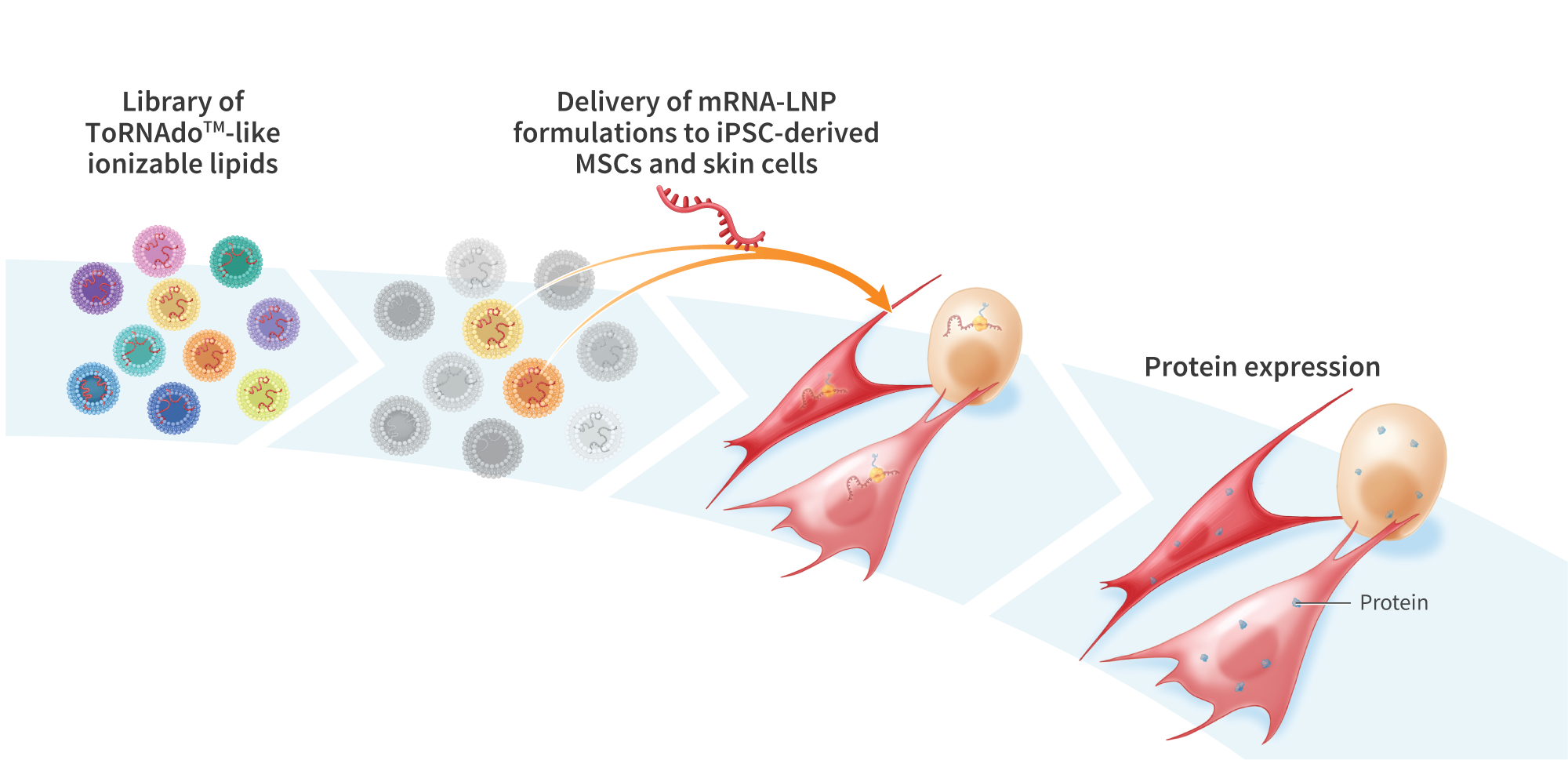
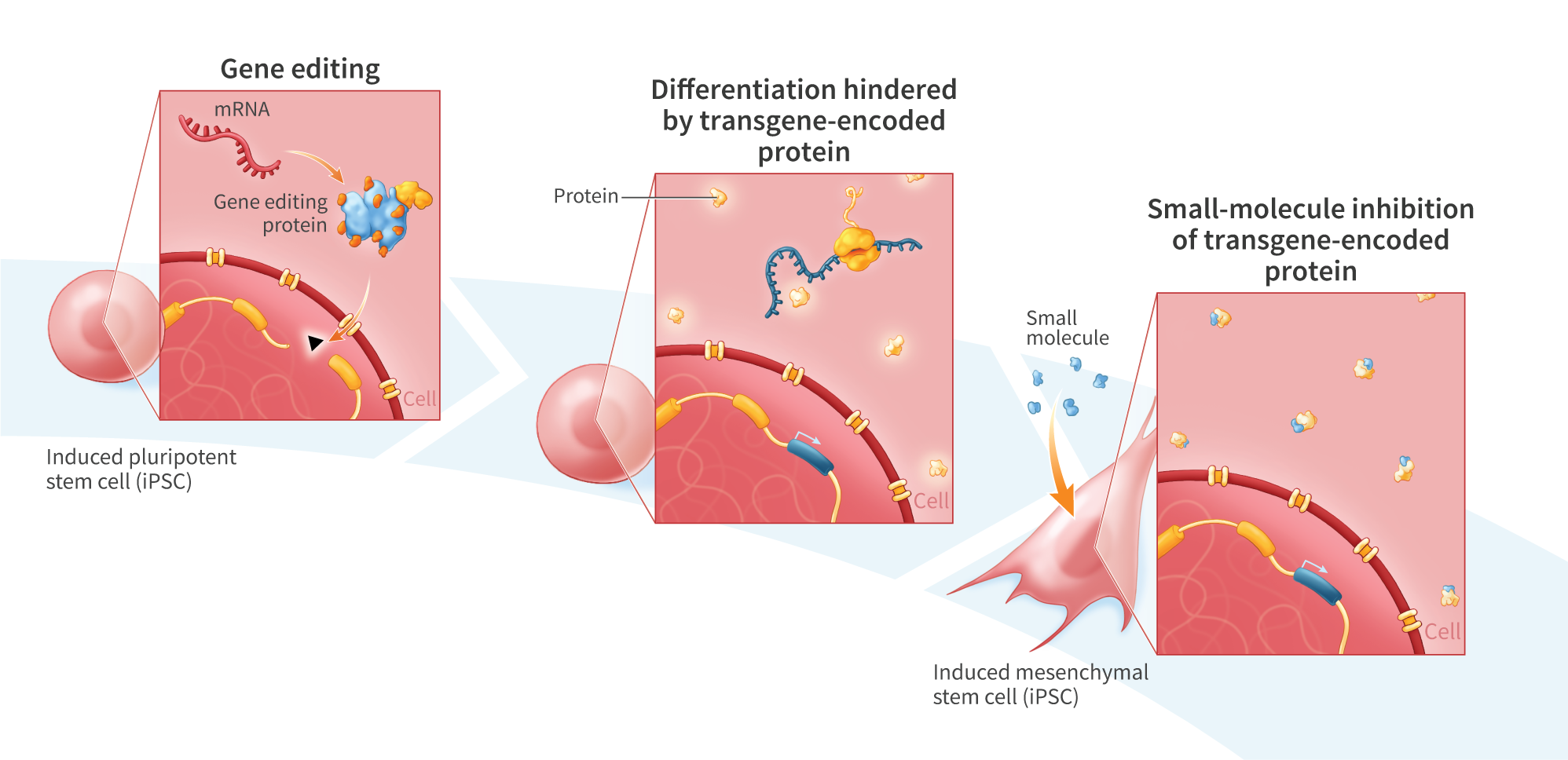
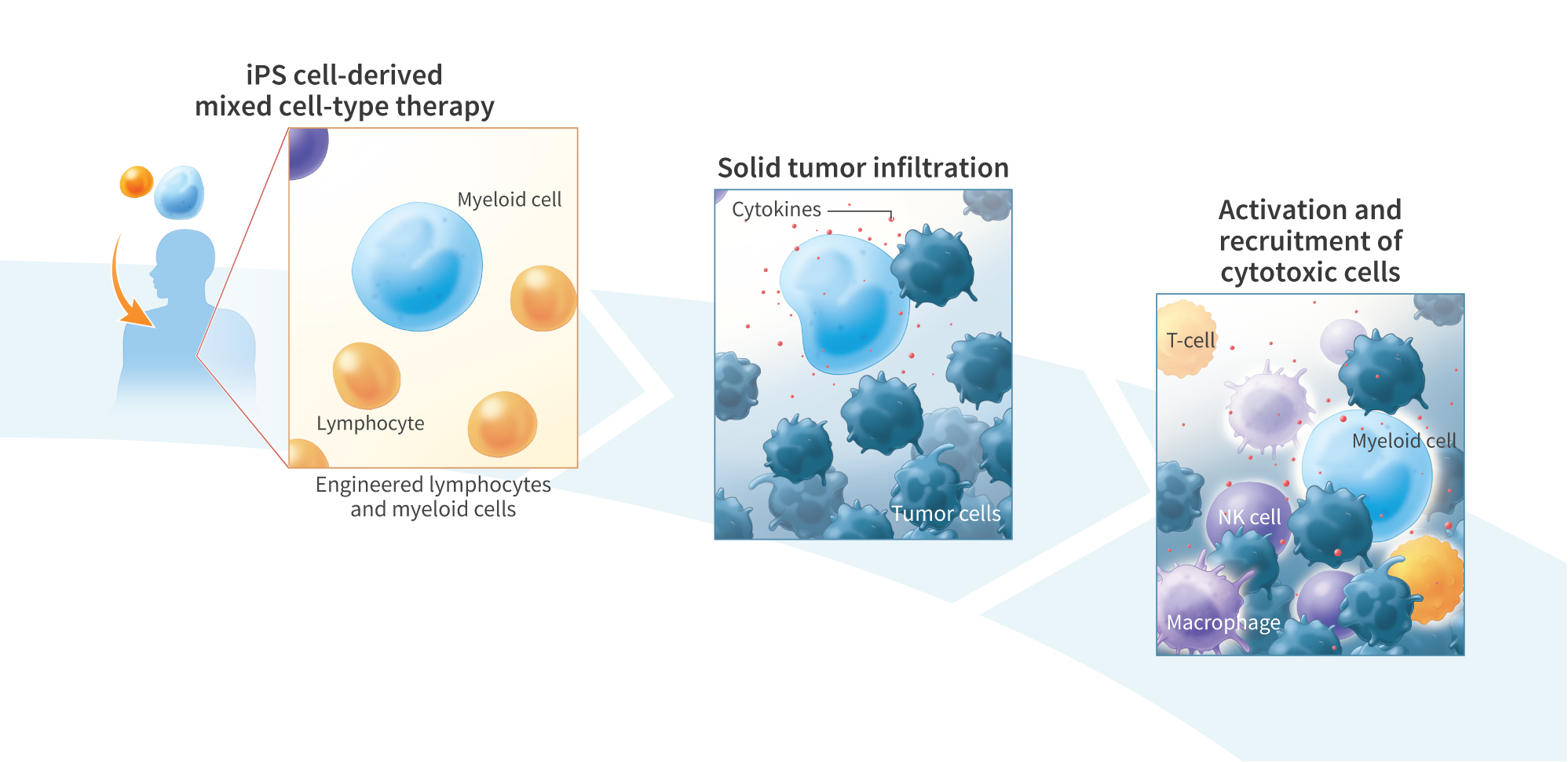
Macrophages’ ability to infiltrate solid tumors and engage in both direct killing of cancer cells and recruitment of other immune cells has made them a promising target for development of next-generation cancer immunotherapies. The innate ability of macrophages to ingest foreign genetic material also facilitates their engineering with formulated nucleic acids, including mRNA. The oncoantigen tyrosine-protein kinase transmembrane receptor ROR1 has garnered interest for its minimal expression in healthy adult cells and overexpression in many malignancies, including solid tumors associated with ovarian, lung, and triple- negative breast cancer. Here, we present an mRNA-based platform for rapid prototyping of macrophage engineering approaches. We show mRNA delivery to peripheral blood mononuclear cell (PBMC) and iPS$ cell-derived macrophages for gene editing prototyping and functional assessment of encoded proteins. To develop this platform, we transfected macrophages with unmodified or 5-methoxyuridine (5-moU)-containing mRNA encoding green fluorescent protein (GFP). Both mRNAs resulted in more than 95% of cells displaying GFP within 4 hours. We next designed an RORI-targeting CAR with a CD3 zeta activation domain and 4-1BB costimulatory domain. Transfection of mRNA encoding the ROR1-CAR yielded 70% CAR-expressing cells, as measured using PE-labelled ROR1. We then compared ROR1 affinity of rabbit and humanized binding domains and found that the humanized binding domain displayed a 2.5-fold increase in affinity as measured by flow cytometry using PE-labelled ROR1. The human receptor domain, but not the rabbit domain, demonstrated activation when bound to RORI1 as assessed by immunofluorescence of CD3 zeta phosphorylation. We also assessed the mRNA-encoded RORI-CAR’s functionality by measuring killing of ROR1-expressing SKOV-3 ovarian cancer cells. Both the rabbit and humanized ROR1 domains of the CAR displayed significantly increased cytotoxicity towards SKOV-3 cells when compared with untransfected macrophages after a 24- hour co-culture at a 5:1 effector-to-target ratio (p<0.01). We theninserted the ROR1-CAR sequence into the AAVSI safe harbor locus of iPS cells under the control of an SFC promotor, isolated5 biallelic-inserted lines, and differentiated them into macrophages. These results demonstrate an mRNA-based platform for rapid prototyping of macrophage engineering approaches. Transfection of macrophages with mRNA encoding a chimeric antigen receptor (CAR) targeting ROR1 resulted in functional expression in vitro, facilitating optimization of the antibody and co-stimulatory domains to improve protein binding affinity and immune activation. This platform thus enables the assessment and validation of novel macrophage gene editing strategies and is being explored for the development of macrophage-engineering therapies for solid tumor applications.